Neonatal Asphyxia Project
Mission
To design a device that applies hypothermia therapy to mitigate the effects of birth asphyxia in neonates born in low-resource communities.
Background
The Neonatal Asphyxia Project (NAP) was launched in late 2015 at the University of Michigan in response to the need for an accessible neonatal asphyxia treatment device. We are a multidisciplinary team of 12 undergraduate students working together with our community partner to address this need in a way that is socially, culturally, economically, and environmentally sustainable.
Neonatal asphyxia is a leading cause of neonatal death in India [1]. The disease manifests during or shortly after birth and can be caused by maternal preeclampsia, infant heart or lung malformations, inadequate oxygenation of maternal blood, knotting of umbilical cord around the infant’s neck, or prolonged delivery. It occurs from oxygen deprivation during birth, and survivors are at risk for developmental delays, disabilities, cerebral palsy, motor disorders, and other physical maladies [2][3][4].
Hypothermia therapy is the standard treatment for asphyxiated infants; by lowering the neonate’s core body temperature by three to four degrees Celcius for 72 hours after birth, hypothermia therapy is shown to reduce the extent of brain injury [5][6][7].
Travel
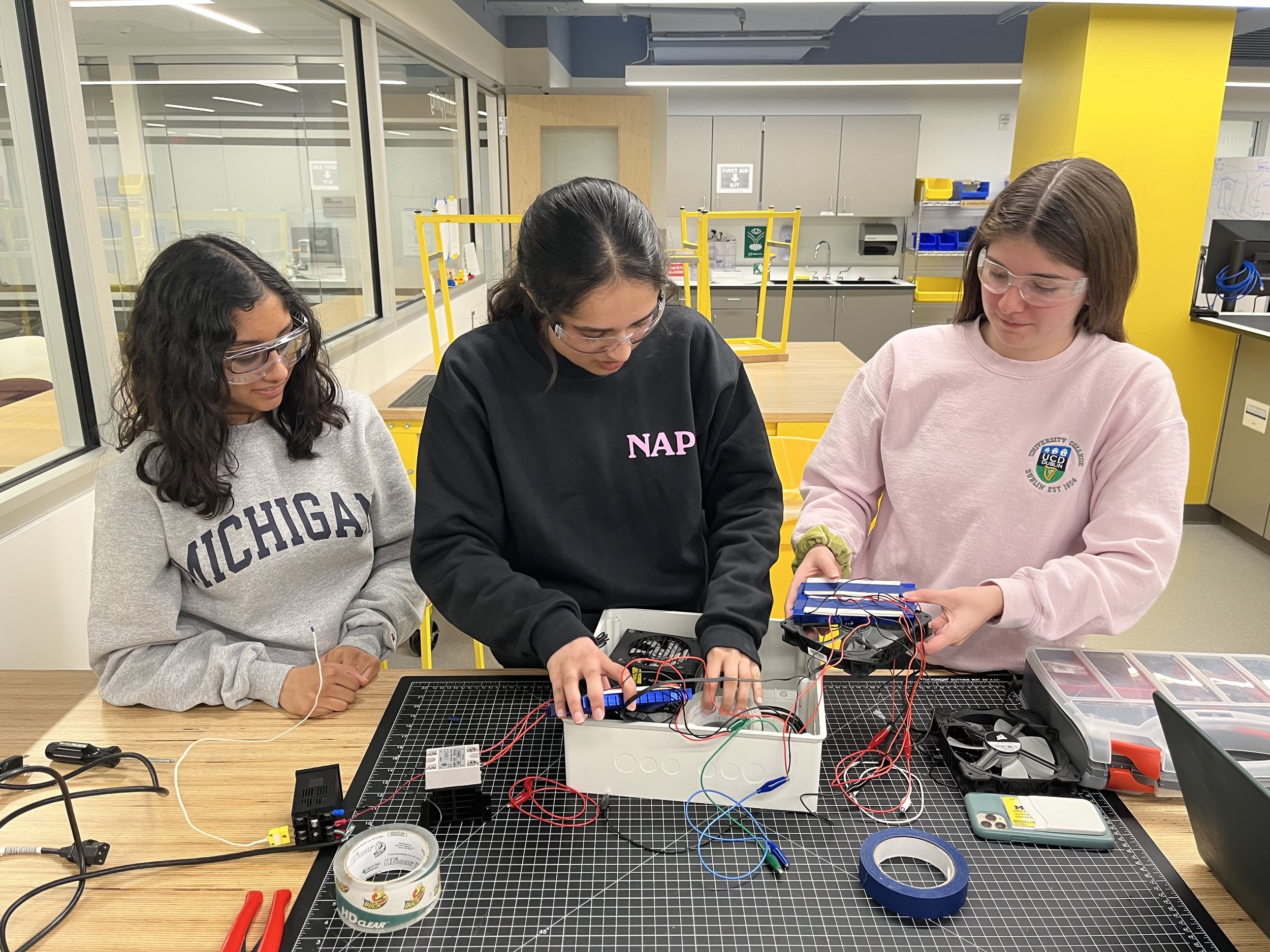
In May of 2023, the NAP team traveled to Palanpur, Gujarat, India to visit our community partner, the Hasya Newborn Care Center.
Testimonials:
“Being able to meet and interact with Dr. Patel and his team at the Hasya Newborn Care Center, as well as seeing our device in its proper clinical setting made our entire project that much more real. We were able to walk through the NICU and see the infants who would benefit from our work, and I’m so excited to see the future of this device.” - Tarana, Business Subteam
“We were able to conduct verification testing protocols for our hypothermia therapy cooling prototype as well as engage with the Hasya Newborn Care Centre in person for the first time in team history.” - Audrey, Team Lead
Awards
2024 Rice360 Global Design Competition Semifinalist
2025 Center of Global Health Equity Competition Finalist
2019 Socially Engaged Design Award
NAP was awarded the First Place Socially Engaged Design Award at the Winter 2019 Michigan Engineering Design Expo. This award “recognizes design teams that demonstrate substantial attention to social, cultural, economic, and environmental contexts in their design process and presentation.
2017 HIE Help Center Scholarship
NAP was awarded the first annual HIE Help Center Scholarship from the HIE Help Center in Bloomfield, MI for our work in designing an affordable treatment device for hypoxic-ischemic encephalopathy (HIE).
Project Members
Team Advisor
Dr. Melissa Wrobel holds a Ph.D. and M.S. in Biomedical Engineering from Wayne State University, where her research focused on biomaterials for nerve regeneration and neural tissue engineering. She is currently a Lecturer IV in Biomedical Engineering at the University of Michigan, where she teaches communication in technical and engineering contexts. Her current education research explores cooperative learning environments, inclusive teaching practices, peer feedback, oral communication, and novel assessment methods. Since 2019, Dr. Wrobel has been a dedicated faculty advisor with NAP, leading our Multidisciplinary Design Program (MDP) efforts with energy and expertise.
Sources
[1] Million Death Study Collaborators et al. “Causes of neonatal and child mortality in India: a nationally representative mortality survey.” Lancet (London, England) vol. 376,9755 (2010): 1853-60. doi:10.1016/S0140-6736(10)61461-4
[2] Kurinczuk, Jennifer J. Epidemiology of neonatal encephalopathy and hypoxic–ischaemic encephalopathy, Early Human Development, Volume 86, Issue 6, June 2010, https://www.ncbi.nlm.nih.gov/pubmed/20554402.
[3] Ahearne, C. E., Boylan, G. B., & Murray, D. M. (2016). Short and long term prognosis in perinatal asphyxia: An update. World Journal of Clinical Pediatrics, 5(1), 67–74. http://doi.org/10.5409/wjcp.v5.i1.67
[4] Halloran, D.R. et al. (2009). Birth asphyxia survivors in a developing country. Journal of Perinatology 29, 243-249. doi: 10.1038/jp.2008.192
[5]Cornette L. Therapeutic hypothermia in neonatal asphyxia. Facts, Views & Vision in ObGyn. 2012;4(2):133-139.
[6] ABC Law Centers. (n.d.). Hypothermia Therapy [How Does Hypothermia Therapy Work?]. Retrieved from http://www.abclawcenters.com/wp-content/uploads/2017/04/Hypothermia-Therapy-copy.png
[7] Lemyre, Brigitte, and Vann Chau. "Hypothermia for newborns with hypoxic-ischemic encephalopathy." Canadian Pediatric Society, Canadian Pediatric Society, 12 June 2018, www.cps.ca/en/documents/position/hypothermia-for-newborns.